Introduction:
Pharmacovigilance, a crucial aspect of the healthcare sector, plays a vital role in ensuring the safety and efficacy of medicinal products. It is a practice that has been in place for about 170 years in the medical industry.
Today this acts as a benchmark for all Pharmaceutical companies to live up to. The Good Pharmacovigilance Practices i.e. the GVP standards are monitored for regulatory compliance to safeguard patient health throughout the drug’s lifecycle.
So what exactly is pharmacovigilance?
What is Pharmacovigilance?
Pharmacovigilance (PV) is the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems.
The European Union (EU) defines pharmacovigilance (PV) as the “process and science of monitoring the safety of medicines and taking action to reduce the risks and increase the benefits of medicines.”
On the other hand, the World Health Organization (WHO) defines PV as “the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problem.”
Initially, PV guidelines were intended to achieve 3 major goals i.e.good quality; efficacy of the medicinal product; and safety for the intended purpose(s).
Later the WHO broadened the scope to ensure occurrences of the following are reduced:
- Interactions of medicines
- Medication errors
- Adverse drug reactions/events
- Lack of efficacy
- Abuse and misuse of medicines
- Counterfeit medicines
Today, the pharmaceutical & life science industry has a set of standardized practices called the Good Pharmacovigilance Practices (GVP), to achieve the goals of pharmacovigilance.
What are Good Pharmacovigilance Practices?
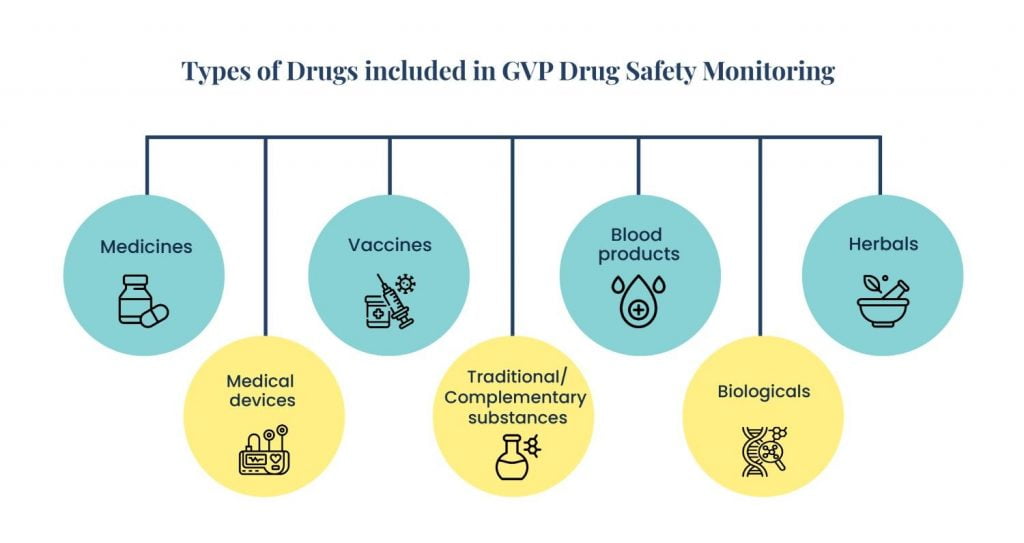
Good Pharmacovigilance Practices (GVP) are a set of measures and guidelines established by the European Medicines Agency (EMA) to ensure the safety and efficacy of medicinal products throughout their lifecycle. GVP focuses on identifying, assessing, preventing and mitigating risks associated with pharmaceutical products, thereby protecting patients from adverse drug reactions (ADRs) and other drug-related issues.

These drugs can be,
- Medicines
- Vaccines
- Blood products
- Medical devices
- Biologicals
- Herbals
- Traditional/Complementary substances
So how do Good Pharmacovigilance Practices (GVP) help in Drug Safety Monitoring? Let’s find out.
How GVP Helps in Drug Safety Monitoring
Good Pharmacovigilance Practices provide a structured and systematic approach to drug safety monitoring. Here’s how GVP enhances drug safety:
1. Risk Management:
- Development of Risk Management Plans (RMPs)
Good Pharmacovigilance Practices (GVP) mandates detailed RMPs for each medicinal product. These plans outline known risks and propose measures to prevent or mitigate them.
- Proactive Risk Mitigation
By identifying potential risks early, pharmaceutical companies can implement strategies to minimize adverse effects before they become significant issues.
2. Signal Detection and Analysis:
- Continuous Monitoring
Good Pharmacovigilance Practices (GVP) require continuous surveillance of data sources such as clinical trials, spontaneous adverse event reports, medical literature, and patient registries to detect new safety signals.
- Signal Evaluation
Once a potential safety signal is identified, it is thoroughly evaluated to determine if it represents a real risk. This involves analyzing patterns and the likelihood that the drug caused the observed adverse events.
3. Collection and Management of Data:
- Comprehensive Data Gathering
Good Pharmacovigilance Practices ensure that all relevant data is collected systematically from various sources, including healthcare professionals, patients, and scientific literature.
- Centralized Databases
These centralized databases are used for storing and managing data. These centralized management practices help in efficient data retrieval and analysis.
4. Benefit-Risk Assessment:
- Ongoing Assessment
Good Pharmacovigilance Practices require continuous assessment of the benefit-risk profile of a drug throughout its lifecycle. This ensures that any emerging risks are weighed against the benefits of the drugs.
- Informed Decision Making
The continuous evaluation process helps regulatory authorities and pharmaceutical companies make informed decisions about the need for regulatory actions. This can include label changes, additional warnings, or even withdrawal of the product from the market.
5. Regulatory Reporting:
- Periodic Safety Update Reports (PSURs)
Good Pharmacovigilance Practices guidelines mandate the regular submission of PSURs to regulatory authorities. These reports provide a comprehensive review of the drug’s safety profile, including any new risks identified and actions taken.
- Compliance with Regulations
Adhering to GVP audits ensures compliance with national and international regulatory requirements, which helps in maintaining market authorization.
6. Risk Communication:
- Transparent Communication
Good Pharmacovigilance Practices emphasize clear and effective communication of drug risks to healthcare professionals, patients, and the public. This includes updates to product labeling, patient information leaflets, and direct healthcare professional communications (DHPCs).
- Educational Initiatives
Providing educational materials and training sessions to healthcare providers ensures they are well informed about the risks and safe use of medicinal products.
7. Quality Assurance:
- Implementation of Quality Systems
Good Pharmacovigilance Practices require the establishment of robust quality management systems to ensure all PV activities are conducted efficiently and consistently.
- Regular Audits and Inspections
Routine audits and inspections of PV systems help identify areas for improvement and ensure compliance with Good Pharmacovigilance Practices standards.
8. Post-Market Surveillance:
- Long-Term Monitoring
Good Pharmacovigilance Practices emphasize the importance of post-market surveillance to monitor the safety of a medicine after it has been approved and is widely used in the population.
- Real-World Data Utilization
Utilizing real-world data from electronic health records, patient registries, and other sources helps in understanding the long-term safety and efficacy of medical products in diverse patient populations.
Conclusion
GVP provides a structured and systematic approach to drug safety monitoring, ensuring that all potential risks are identified, assessed, and managed throughout the lifecycle of a medicinal product. By adhering to Good Pharmacovigilance Practices, pharmaceutical companies can enhance patient safety, maintain regulatory compliance, and build trust with healthcare providers and patients.
